Introduction:
14.11.25.
40 typical images demonstrated 3 basic rules in radiology:
summation-, silhouette phenomenon and shell-sign.
The importance of those rules for diagnosis of pneumothorax and
pleural effusion and fibrothorax (with and without calcification) are clearly depicted. Special attention is paid to tension pneumothorax, to
distinctive variability in forms of effusions and to special methods.
The typical effects of a fibrothorax are shown:
– volume-reduced hemithoraxup to compression-atelektasis
– distortion of the heart / mediastinum, thickening of the ribs,
– intercostal narrowing (excessively), scoliosis, deformation of the ribs.
The importance of detecting persistent effusions between both calcified pleural layers, most often a chronical emyema has been pointed out.
Differentiation of the lesion metioned against peumonia and atelektasis has also been visualized in numerous examples.. –
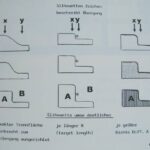
Cases 1-5 summation-, silhouette phenomenon
- There are 3 basic rules in radiology:
summation-, silhouette phenomenon and shell-sign.
Ultimately, we want contrast. If all rays attenuate at the same level, this results in a homogenous grey area, which means a complete lack of contrast.
We want ‘ray X’ and ‘ray Y’ to be weakened differently.
Let us assume the following: the body to be examined should consist of 2 substances (A and B).
Left part of drawing: the thicker A is, the more ray X is attenuated (in comparison to ray Y);
picture 1:
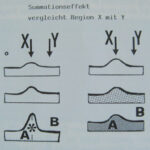
The Summation Phenomenon.
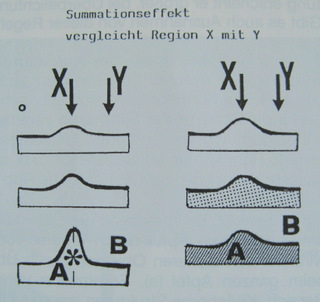
The body to be examined should consist of 2 substances (A and B)
What is shown in the right part of the drawing?
(Click here for the answer)
For the purpose of argument, let us suppose that the geometry we have is totally stable.
The greater the density difference between A and B
To be physically precise, we determine that it is not only the density but also the (effective) atomic number which has to be considered.
To conclude: the rule is simple. The thicker and/or denser the object is, the greater the attenuation of radiation. This corresponds to a less bright region in the film. We call this “opacity”, the opposite of “translucency”. –
In German it is rather more complicated:
a bright structure in the radiograph (e.g. a pleural effusion) is termed “Verschattung”; a dark structure (e.g. a pneumothorax) is referred to as “Aufhellung”. This paradox results from fluoroscopy where information provided is inverse: “black” in the image is transparent on a fluoroscopy screen; “transparent” in fluoroscopy is “black” on the x-ray film.
picture 2:
An interesting riddle inspired by Pantoja. What is changed about the material “apple”?
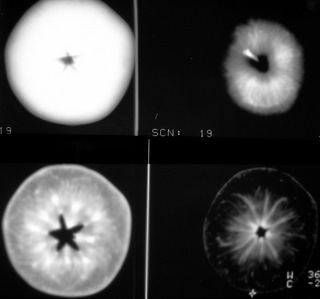
Here are 4 x-rays of objects and all have been obtained under the same conditions:
same kilovolt (KV),
same mAs,
same distance,
same intensification factor,
same material!
What material is it, and what has (obviously) been changed within the object?
Material is “apple”
Thickness has been altered by cutting the apple.
Top left: the whole apple
Bottom Right: just a slice of the apple
A slice is of an apple is transparent (less summation) We see in the slice more details because not too many details are superimposed! But the disadvantage is that there is only one slice, all the other slices are not been recorded.
Truth be told, this is not a regular x-ray; but a composition of CT-slices. A summation of slices can simulate an x-ray precisely. The summarizing (“averaging” is a little different) of a “CT- examination of head” provides one with a nice x-ray of the skull. X-rays of those objects look exactly the same. To experiment and to photograph is much easier in digital conditions.
3. In what field of radiology is the term “Silhouette” best known?
“Silhouette sign” is well known in thoracic radiology. Heart and diaphragm have clear silhouettes (A = soft tissue, B = air containing lung). Pneumonia leads to a loss of cardiac or diaphragmatic margins, depending on where the change in pulmonary parenchyma is located.
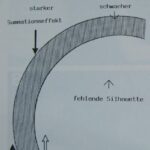
The sign we want to talk about now, deals with the contours, edges, or margins.
The less parallel the border area runs, the more lost, or more imperfect, becomes the delineation sharpness. If this delineation runs very obliquely or perpendicular fashion to the beam path, it is impossible to visualize it.
picture 3:
“Silhouette sign”
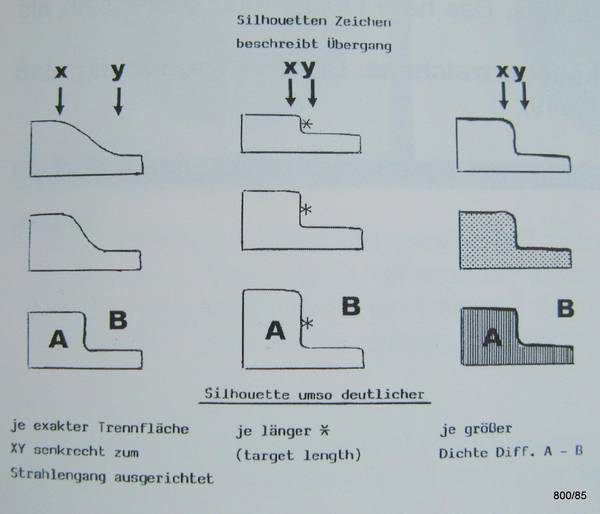
What do the middle and the right images show?
In good geometry the silhouettes are clearer when the thickness difference from A to B is greater (middle).
– Silhouettes are even better, if the density difference of A to B is greater (right).
- they are better if the target length – marked with the star – is larger. –
- And it is better if the target length is aligned more precisely with the beam path (the German text in the figure below left “senkrecht zum Strahlengang”) is ambiguous)
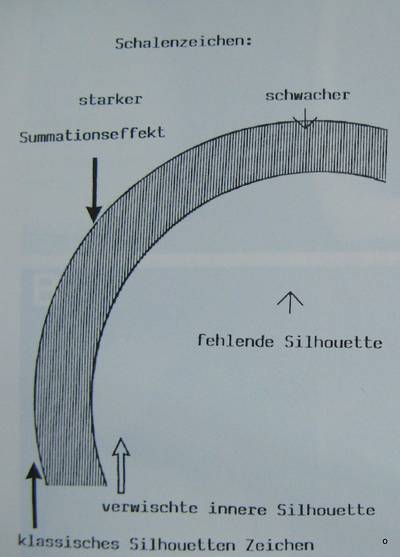
- This is a special case of silhouette phenomenon: a shell of dense material causes a silhouette on its outer and inner shape.
A snail’s outer shell shown here creates a remarkable x-ray. Not only the outer but the inner surfaces are visualized in some parts of the x-ray film. It demonstrates the strengths of the Roentgen method.
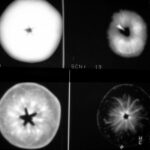
picture 4:
Shell Phenomenon
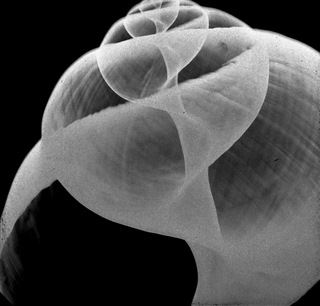
Why are the weaknesses also shown?
The shells are everywhere delineated as being razor-sharp, where they are tangentially projected. Where, however, the shell is taken in perpendicular manner (pictured in the bottom left corner), this produces a low or no “shadow” area. We are unsure whether or not a wall exists in that region.
5. There are plenty of shell-like structures in anatomy and pathology.
picture 5:
pleural calcification.
Here is one example of calcification in the pleura diaphragmatica.What is the difference between the two pictures? Why is the presentation so different?
5. There are plenty of shell-like structures in anatomy and pathology.
Cases 6-10 shell-sign
6. In the tangential way the passage of rays is 7 folds in length, in comparison to the perpendicular passage. Longer passage means more intense attenuation, and results in better visualization.
picture 6: weak and dull imaging of the shell: heavy and light Summation
picture 7: First object. This is an x-ray of what?

picture 8: A ball of silver paper: this paper is only visualized where it is positioned parallel to the beam.

Remark Picture 6: The path of a tangential beam is approximately seven times longer than that of a radial beam.
7: open book.
What happens in tangential projection?
There the radiation is significantly attenuated and this attenuation results in sharp lines.
picture 9: How can you explain this “x-ray” with the hypothesis that “every radiograph of an object is the sum of all its slices”?
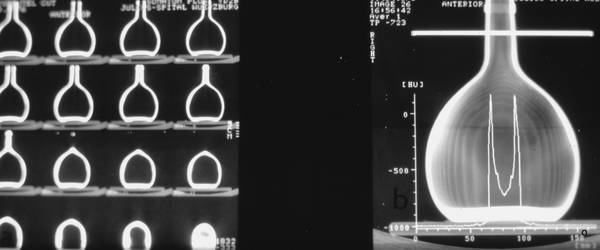
We see the slices in the left part of the image. Summarizing the slices, the ventral and dorsal wall is only added twice; the edge contours are added a dozen times or more. Therefore, the edge contours dominate.
9. Right part:
picture 10: Diagnosis? Why is it difficult or impossible to observe this pathology in the summation-radiography (in the usual X-ray image)?
Calcified fibrothorax on both sides of dorso-medial pleura. – Calcification is not projected tangentially and subsequently overlooked in the standard (posterior-anterior) radiograph. (A tiny calcification on the lateral right side is only detectable though very careful observation).
Cases 11-15 pleural calcification, pneumothorax
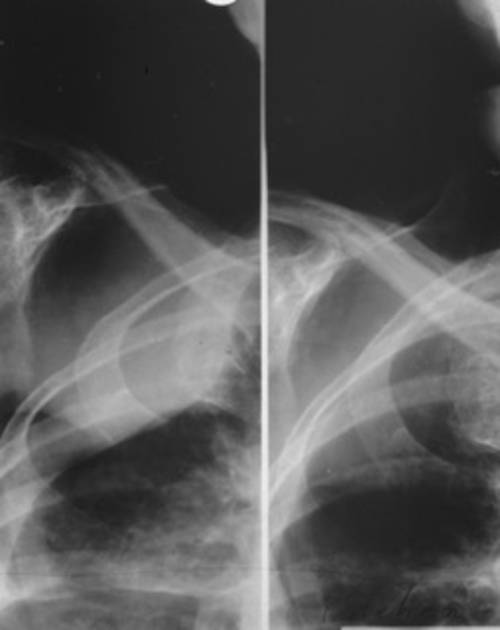
picture 11: How is the chest rotated?

Left: the more you see ventral ribs, the more it is an LAO projection! Calc.1 is far dorsal.
Middle: typical pa projection. “2” is the dorsal border of the calcification.
Right: ribs seem to fall from medial to lateral. The lateral shape of ribs is ring-like. This is typical for RAO projection (of a left hemithorax). – “3” is a calcification far ventral.
picture 12: Diagnosis is pneumothorax.

What can we actually see of the two pleural leaves and the pleural gap in a healthy individual?
When healthy, we don’t see anything of the pleural leaves or pleural gap. Only when the gap is extended (as it is here by air or liquid), will it be visualized. There is even a relatively great contrast between a compression of the lungs (positive summation-effect) and
pneumothorax (negative summation-effect).
The visceral pleura thus forms a well visible silhouette; here it is marked by black dots.
In Dutch, there is a very good word for pneumothorax: ‘klaplong’. This word helps to understand ‘radiodiagnostics’. The lung (covered by the lung membrane) folds in on itself by its own elastic force. However, it can only do this if air has entered between the lung membrane and the pleura.
Normally, there is only a wafer-thin film of fluid in this space. This cannot expand and prevents the lung from ‘collapsing’. Instead, it has to follow the movements of the chest and expand or contract.
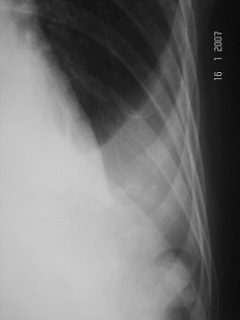
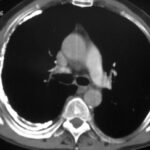
picture 13: Emegency? Diagnosis? Why is this image modality insufficient?

Pneumothorax
If this diagnosis still seems difficult for you, it is necessary to repeat the case shown in picture 12 Could it also be a skin fold, i.e. an artefact? We don’t think so, because the space of the pneumothorax is free of pulmonary vessels, while the lung is clearly structured. A skin fold would also be compacted but less structured.
The clinical question is: does the patient (urgently) need a pleural drainage to ventilate the left lung? In order to answer this, we need to see the whole thorax and assess whether the heart and mediastinum have been shifted to the right.
“Tension-pneumothorax” requires prompt action!
In one case (13) the space contains air, and in the other (14, 15) an effusion. Characteristic of the effusion is the homogeneous shadowing close to the thoracic wall.
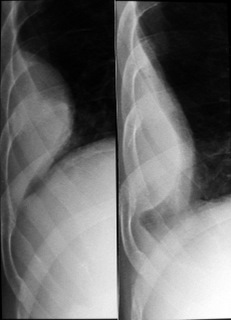
picture 14

What difference may we draw between an effusion and a soft tissue process (e.g. mesothelioma or peripheral bronchial carcinoma)?
Pleural effusions are often characterized by form mutability depending on body position. The two picture shows the change between prone and supine. Sonography is even more important here; it shows the transonic fluid and its deformation depending on body – and diaphragmal position (respiration).
In CT contrast medium intravenously gives direct evidence of tissue perfusion. Tumours will enhance, effusion will not.
picture 15
Is there a definite rule as to how the picture changes in the prone position, or in the side-position?
Unfortunately not. Pleural adhesions can sometimes prevent a typical shift of effusion. Try it wether you see a typical change. Sonography will help to solve the problem.
Do you agree so far?
Cases 16-20 pleural effusion
picture 16. Two very similar projections; same time, same patient.
What is the difference? How can it be explained?
Pleural effusion: left = prone, right = standing up.
We may also demonstrate those effects also by means of sonography.
picture 17. Pleural process? How are the two pictures achieved?
Difference in diaphragm position proves it is expiration (left) and inspiration (right). Partly encapsulated effusion considerably deforms with breathing.
picture 18: Same patient. What technique is applied here?

Subtraction of in- and expiration. It demonstrates diaphragmal mobility and form instability of the mass lesion. This mobility is a good argument for “encapsulated effusion”.
picture 19
One form of pleural effusion often overlooked: the “subpulmonal” effusion, which (as an exception) we see here very clearly. Why?
There is free air in the abdomen caused by gastric perforation. This thin layer of air causes a (caudal) silhouette of the diaphragm. Thus the thick layer between diaphragm and lung will be a subpulmonal effusion.
picture 20

Diagnosis? What do the black points show?
A dark line, difficult to pick out, corresponds to paradiaphragmal fat. This gives us an idea of the diaphragm position and of the effusion on top of it:
basal = subpulmonal effusion.
Cases 21-25 special findings in effusions
21. Both are the patient’s left hemithorax. (Right part of the picture is turned mirror-like) Between both x-rays the patient received antidiuretic therapy.
picture 21: The follow-up hemithoraces, both right! are shown mirror-like.
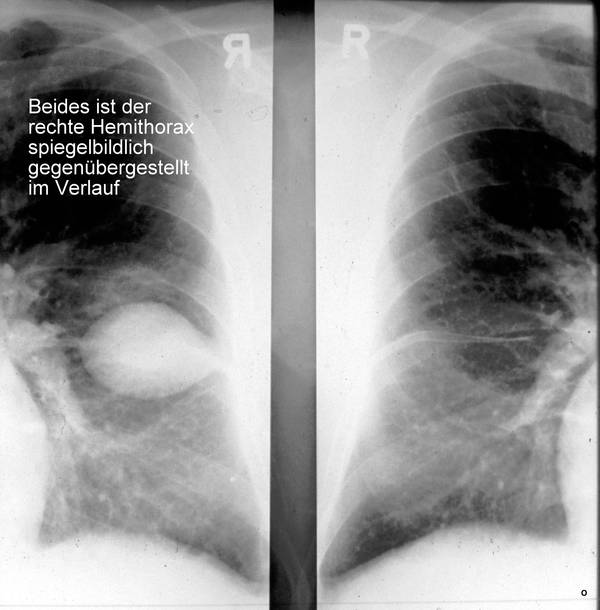
Diagnosis?
Interlobular encapsulated effusion. It disappeared after therapy; the strongest argument against a solid mass.
picture 22. Irregular homogeneous masses in the neighbourhood of the chest wall and the mediastinum? No known malignant disease but. several pneumonias. Probable Diagnosis?
Encapsulated effusion. The pleural space is a drawing of a life story. Multiple bonds often exist. Many kinds of pathology vary in shape and manifestation. (Normal anatomy does not show so many variations as pathology does). At this point in time, the cause of the effusion was still unclear.
picture 23. What is the technique in this case? Which are the findings?
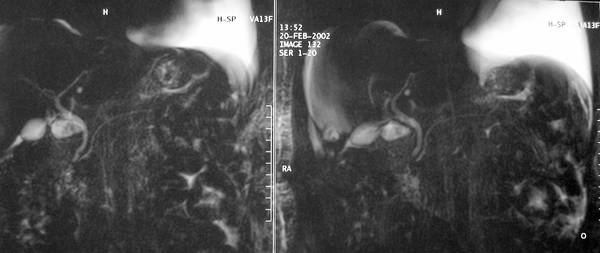
Magnetic Resonance Tomography (MRT): Liquid appears light; T2 weighted; no pathology of bile and pancreatic ducts. In the upper right quadrant of both images homogeneous fluid = pleural effusion. This was an incidental finding.
24. In sonography findings are typicaly dependent on
- body position,
- diaphragmal position and the
- reaction produced by percussion. –
picture 24: The important Sonography of pleura
Does this image contain an atypical finding?
It is inverted. The transonic effusion – shown here lightly – is black in the usual procedure and setting.
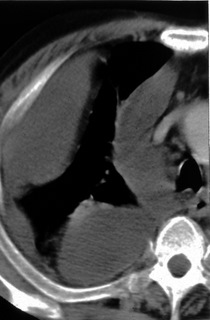
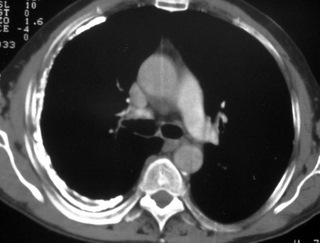
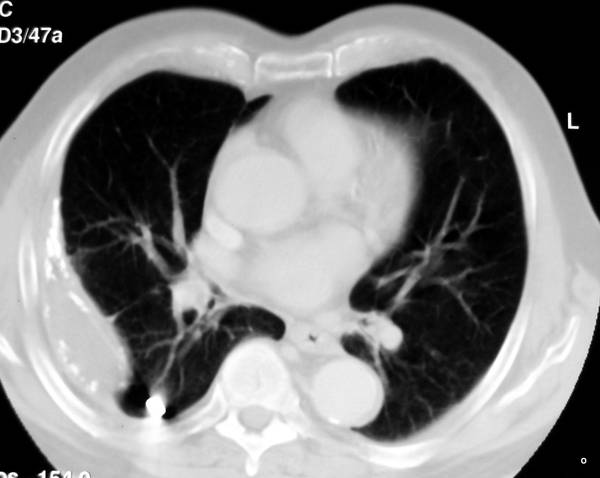
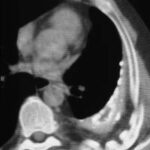
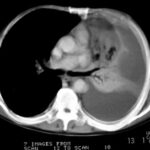
picture 25 Pleural effusions with CT; twice the same slice
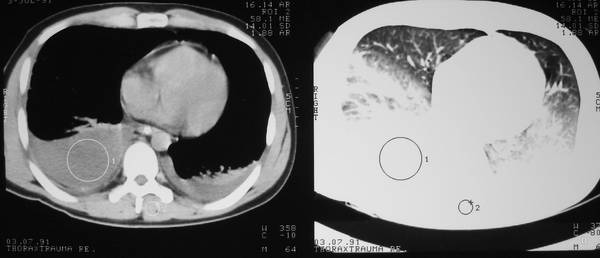
What has changed? What should be demonstrated? Same slice, 2 different displays.
Effusion results in a restrictive lung lesion. Effusion always means (more or less) compression atelektasis. The moderate atelektasis is missed in the soft-tissue window (left), but shown clearly in the lung window. “A window” translates the “density” numbers (according to Housfield = HU) in an optical black-and-white scale.
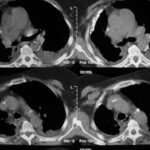
26. Everyone knows the causes but also the effects of effusions. It is an aggressive effusion in this case. Which effect is further demonstrated here? Tension effusion
(analogous to tension pneumothorax) shifts the mediastinum to the left; most recognizable by the contrast-enhanced ascending aorta, which is usually right of the midline. Total atelektasis of the lungs.
picture 26. What are the black ties within the compressed lung?
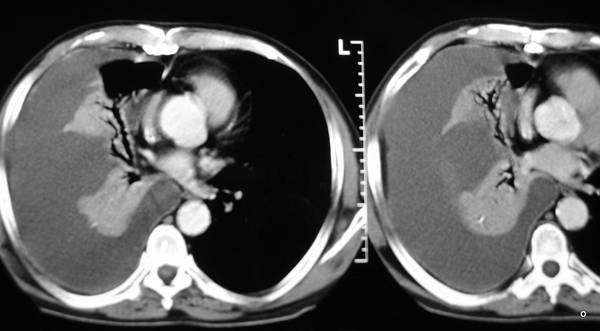
Air containing airways = positive aerobronchography.
Cases 26-30 effusion, peumonia or pneumothorax
27. Can we see signs of “positive aerobronchography” in other entities? We may detect this sign most commonly in cases of pneumonia; in an estimated half of all pneumoniae. –
It is pneumonia in this case.
But the phenomenon is also found in the compression-atelektasis as shown in case study number 26 above. It is not found in obturation-atelektasis as it is produced by a bronchial carcinoma). In this patient we find a shadow (X-ray diagnosis) produced by a pneumonia (pathological diagnosis).
picture 27. Why does “positive aerobronchography” sometimes consist partly of “black” points and partly in “grey” ties?

Black dots are bronchi running in the direction of radiation; dark grey stripes are bronchi taken from a vertical (perpendicular) perspective.
picture 28
Back to the main topic: pneumothorax and/or effusion? Both are sometimes of little clinical significance. Should it be neglected here?
No! In this case it is an emergency. “Pneu” (in this case) and effusion become dangerous if they shift the heart and/or mediastinum! Here is a tension pneumothorax: significant enlargement of the left chest cavity, total collapse of the lung and (until now) only moderate dislocation of the heart and mediastinum to the right. Can increase soon! Emergency!
picture 29

Repetition: CT shows you an effusion. Can you pick out all of the three x-ray signs, that have already been discussed: “Atelektasis”, “Aerobronchography” and “Mediastinal-shift”?
Yes we can! Despite a small adhesion of the pleurae the lung has collapsed. This compression atelektasis shows typical aerobronchography. The position of bifurcation helps to decide thatthe effusion is space-occupying.
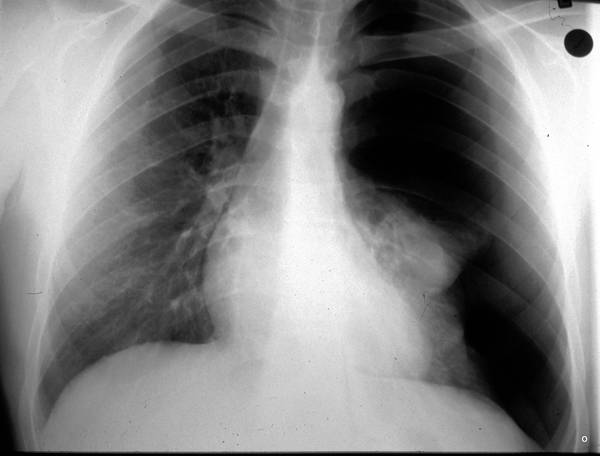
##########################30. Insert of one “non pleural case”. The pathological picture is below. Here we are unable to make a pathological diagnosis, as we know too little. Therefore we can only make a diagnosis based on the X-ray.
Total shading of the left lung. Mediastinum and heart are warped towards the sick side; most obvious is the distortion of the trachea. That is only an X-ray diagnosis.
pictures 30. It is the same patient; 6 hours have passed between the upper and lower image. The shortness of breath has worsened considerably. Asymmetry on percussion and auscultation.
What could be hidden behind this?
It is total atelektasis. This is strongly supported by a high stand of diaphragm and the exclusion of effusion in sonography.
Cases 31-35 effects of fibrothorax
31. Here in this new case we have similar findings (left hemithorax is markedly reduced in size). But the underlying disease is completely different; a long history with long lasting pleurisy; unchanged for many months.
We are back in the pleura: pleural scars can calcify;
extensive pleural scarring = fibrothorax. Of course fibrothorax can calcify. The rules for a post-inflammatory pleural calcification are not clear. The extent of the calcification does not strongly correlate with the degree of restriction! Detection of calcification does not help to clarify the ethiology (bacterial empyema, specific pleurisy, traumatic hemothorax?)..
picture 31. Why is the proof of pleural calcification important?
Calcification is helpful to localise the disease as a pleural disease. It helps to recognize the complications. (This will be demonstrated later in several cases).
Once again: what is the impact of pleural scars? (anatomic view) It is primarily a restrictive impact.
The shrinking of the lung causes:
Restriction of breathing movement,
Reduction of lung volume,
Distortion of the mediastinum,
Distortion of the diaphragm,
Scoliosis,
Thickening of the thoracic ribs (Eyler),
Narrowing intercostal spaces.
Fibrothorax can, as in this case, reach excessive proportions. In plethysmography we find strong restrictive changes.
How does the restrictive impact take shape in this present case?
(Click here for the answer)
Mediastinum strongly warped towards the right; particularly evident in the trachea. Severe reduction of the right thoracic cavity, significant scoliosis, the right ribs are forced into an expiration position, clear thickening of the ribs (compared with the opposite side, see William Eyler and coworkers)!
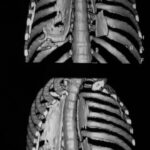
32. a new case of illness with pleural scar. Note the typical uncalcified layer (mostly fat) between calcification and ribs. This layer ensures a degree of mobility of the remaining right lung. Such fatty tissues can arise in various shrinking processes. Restrictive changes are strong and often underestimated. The enthrallment of the lung by pleura causes 8 radiological signs which are quite similar to the anatomical results mentioned above in the last case.picture
picture 32. To reiterate… as mentioned previously:
Calcification of both pleurae. Uncalcified epipleural layer,
Thickening of ribs, (in comparison to opposite side),
Reduction of the thoracic cavity,
Expiration position of the ribs,
Narrowed intercostal space,
Scoliosis,
Mediastinal distortion (here less developed).
If you did not detect so many signs or indications, you should use the next 8 images as room for improvement, otherwise move on to case number 41.
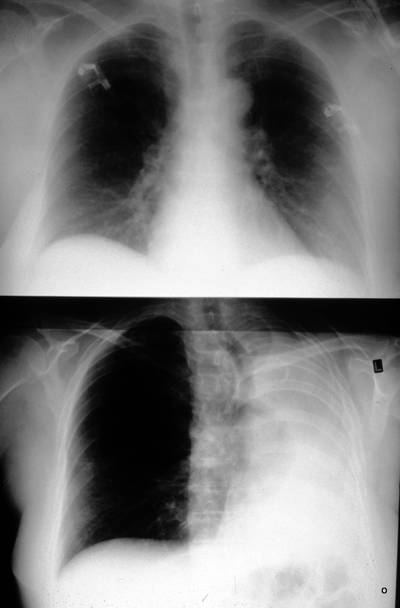
picture 33: Repeat the symptoms of this (mainly) right-sited fibrothorax in this film.

Which of these are more or less pronounced? What could an additional finding be?
Particularly clear is
the following:
- epipleural fat layer,
- elevation of the right diaphragm,
- tracheal shift to the right, the heart remains in its place,
- no statement about rib pathology.
- A splinter is more likely to show the reason of fibrothorax: empyema after splinter injury.
- As a new additional finding: acute pleural effusion to the left; after a minor puncture one finds a mirror Pneu and fluidrest = Seropneumothorax.
picture 34: Again, on the right side a calcified fibrothorax, on the left side a fresh pleural effusion. The pleura can calcify irregularly (but also very evenly).
Shrinking of the right lung and marked shift of the mediastinum to the right. Which of the effects of the fibrothorax are less clear?
The epipleural fat and thickening of the ribs are not clearly demonstrated. This can happen.
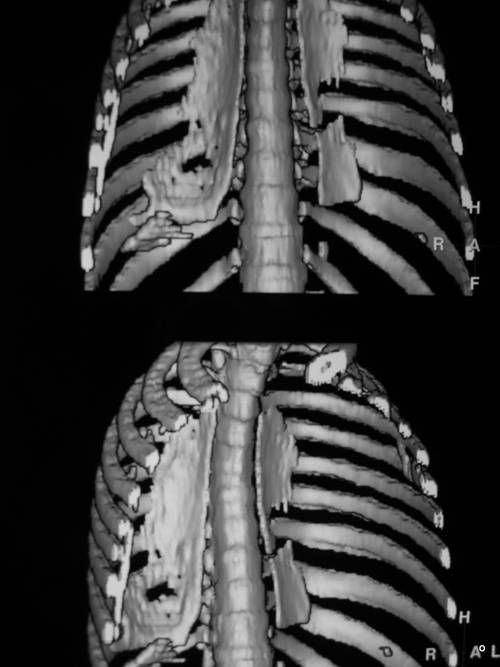
picture 35. another new case of the disease. What is recognizable?

The overview x-ray (below) is underexposed (and was made with loe low KV?) and proper diagnosis is not possible.
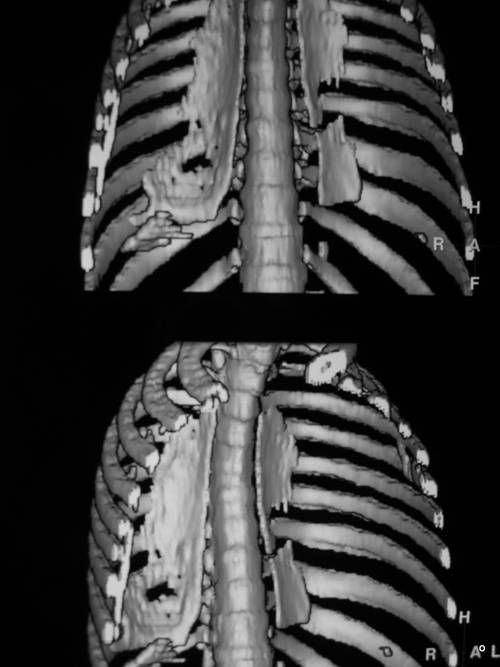
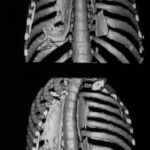
In CT examination – here in the form of a 3D reconstruction – we can see a clearly calcified fibrothorax on both sides. A possible suggestion could be that the location is “untypical”. Do not assume a favourite location of pleural calcification.
Cases 36-40 deeper understanding of pleura
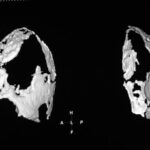
36: 3D surface reconstruction from the CT: the ventral part of the chest has been virtually cut off and we are looking into the left and right chest; inside an extensive, irregular-shaped fibrothorax. There is a distinctive variability in forms (as always in pathological processes).
picture 36. From which direction are we now looking into the thoracic cavity? What we see except vertebral column and ribs?
Upper picture: anterior-posterior/ slightly from the right.
Lower picture: RAO view.
What could we do to eliminate the overlay by ribs and vertebra?
New paIient with pleural calc.. A segmentation has been carried out. The pleural calcification is shown without the bony structures in the surrounding area (ribs and spine). It has little diagnostic importance. In caudal/lateral position the shell is not flat but bulky. That could contain a persisting effusion.picture
picture 37. Segmentation of pleural calc.
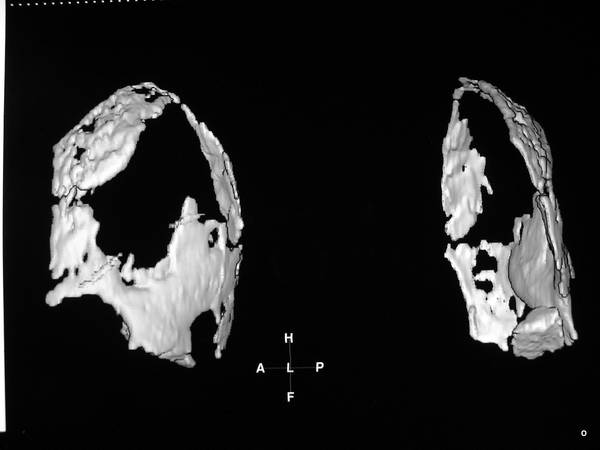
We can’t diagnose it from these pictures! It was diagnosed by ordinary CT-slices and by puncture:
Persistent effusion between both calcified pleural layers;
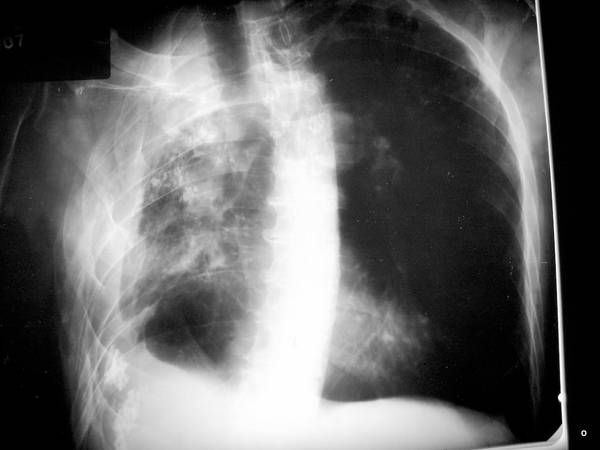
picture 38: Fibrothorax after specific pleurisy.
Which signs are clear? What is distinct? What is new?
Unusually small amount of shrinkage of the right thoracic cavity.
Only minimal distortion of the mediastinum to the right (see bifurcation!).
Remarkable thickening of the ribs on the affected side.
If you remember this sign, you will discover it in the majority of fibrothoraces. It was first described by Eyler and his colleagues (among them the author W. G. H. Schmitt-Buxbaum).
The duplication of the dorsal pleural calcifications is undoubtedly spectacular. It could contain a very small persisting effusion between the two (calcified) pleural layers.
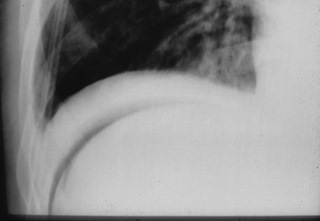
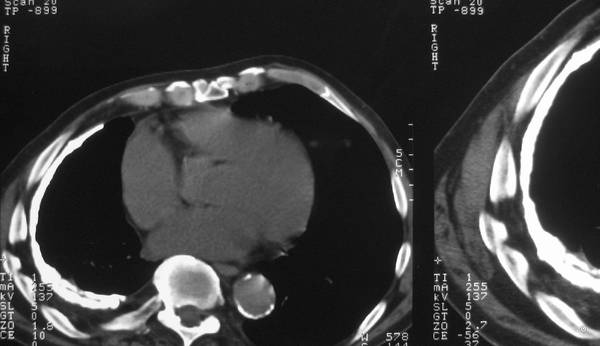
picture 39: Pleural empyema 20 years ago. What is typical? What is particularly strange?

Here we find almost all of the typical effects of a fibrothorax:
-volume-reduced hemithorax,
-distortion of the heart / mediastinum,
-thickening of the ribs,
intercostal narrowing (excessively),
-scoliosis,
-deformation of the ribs (bony apposition exp. on the inner side).
The extensive uncalcified layer between pleural calcification and chest wall (marked by the interior contours of ribs) is characteristic.
In the field of radiology, this layer has caused the biggest misunderstanding of the pleura-topic. In the following we will discuss it in detail.
Srange is a small hypodense area surrounded by scar tissue. It could be a small residual effusion? A very little residual effusion! No clinical signs for inflammation.
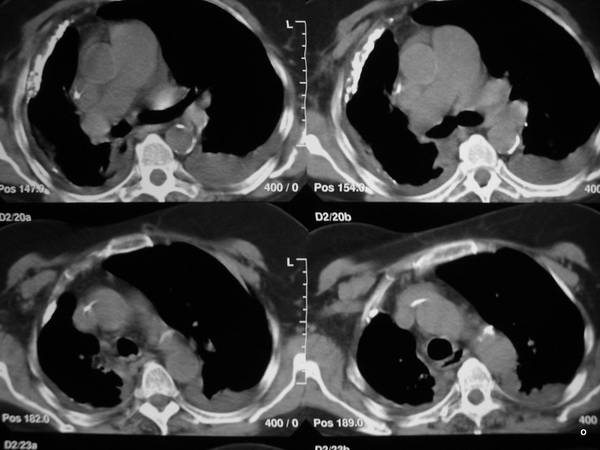
40. We find a dense artefact-producing body close to the suface of the right lung, in contact with a dorsal rib: metal splinters. History of empyema.
There are only a few classical signs of fibrothorax in this case but a separation of both pleurae. We have little doubt there is a cavity with fluid inside. No reaction for years, but we sould observe the patient carefully.
picture 40: History of empyema. Persisting pleural cavity?
We see not one but two calcified layers encasing a homogeneous structure. The patient came with the misdiagnosis of simple scarring. – This could only be an effusion and nothing else. We will prove this in the following text by drawing on a significant number of cases.
More – and I think interesting – Acute and chronical pleural Empyemata in the next presentation. 07 Pleura III.


















1 Comment. Leave new
Is 39 the wrong picture? We find out! Wolfgang