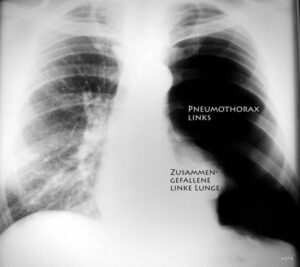
Fall 1. Was ist Ihre Diagnose?
Dies ist eine 41-jährige Frau, die sich vorgenommen hatte, etwas für ihre Gesundheit zu tun.
Sie kaufte sich ein Paar teure Laufschuhe und lief jeden zweiten Tag eine 6,5 km lange Asphaltstrecke in ihrer Heimatstadt. Die ersten Male fielen ihr sehr schwer, aber bald machte sie unter den staunenden Blicken der Nachbarn große Fortschritte. Das motivierte sie, sich noch mehr anzustrengen. Sie war stolz auf ihre Leistung.
Doch genau zwei Wochen später wurde diese Erfolgsgeschichte durch Beschwerden in der rechten Ferse getrübt. Gegen Ende des Laufs steigerten sich die Symptome zu starken Schmerzen in der gesamten Ferse. Selbst in Ruhe war sie nicht mehr beschwerdefrei. Die Patientin versuchte es erneut mit dem Laufen, brach aber – sehr enttäuscht – ab und ließ sich mit dem Auto abholen. Danach machte sie eine Laufpause.
Die Patientin erkannte die Ursache ihrer Beschwerden richtig: „Ich habe es übertrieben – mehr, als mein Körper tragen konnte.“
Aufgrund der Anamnese ist es sehr wahrscheinlich, dass die Verletzung durch Überlastung entstanden ist. Es lag kein akutes Trauma vor, wohl aber eine ungewöhnlich langanhaltende Belastung; die Anamnese weist nicht auf Infektion, Tumor oder Thrombose hin. Der Ausschluss anderer Ursachen lässt uns von einem „Missverhältnis zwischen Belastung und Belastbarkeit“ ausgehen.
Liebe Leser, dies ist der am häufigsten besuchte Fall. Es gibt dazu auch einen weiteren Beitrag: „Ossäre Insuffizienz I“ – weniger MRT, mehr Übersicht über das gesamte Thema.
Die Überlastung des Knochens hat eine verwirrende Vielzahl an Synonymen: Stressfraktur, Marschfraktur. Die vielen verschiedenen Bezeichnungen für dasselbe Phänomen zeigen, wie schwer es die Medizin mit diesem Thema hat. Keine dieser Bezeichnungen ist falsch – sie beschreiben die Entstehung der Erkrankung. Ich bevorzuge den Oberbegriff: „ossäre Insuffizienz“. „Remodeling-Zone“ ist keine Bezeichnung für die Erkrankung, sondern ein auffälliges bildgebendes Symptom. Mehr dazu später.
Die Ursache der Erkrankung ist ein Missverhältnis zwischen Belastung und Widerstandskraft. Das ist übrigens auch die Ursache eines akuten Traumas! Bei unserer Patientin war ein bestimmter Verletzungsmechanismus wirksam: wiederholte kleine Traumen. Diese allein würden keine Verletzung verursachen – erst in Kombination können sie Schäden anrichten. „Chronisches Trauma“ ist logisch gesehen ein weiteres Synonym.
Je nachdem, ob ein wachsender oder reifer Knochen betroffen ist, stellt sich die Schädigung unterschiedlich dar:
Der wachsende Knochen ist besonders empfindlich: die Wachstumsfuge (Apophyse oder Epiphyse) und angrenzende Knochenbereiche.
Beim Erwachsenen ist die größte Anfälligkeit im Bereich der Knochenschäfte. – Beim Calcaneus betrifft es den Corpus (manchmal in der Nähe der Tuberositas, manchmal zentraler).
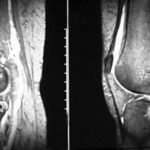
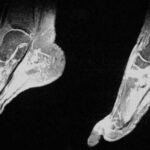
Zwei Tage nach Trainingsstopp zeigte das Röntgenbild noch keine Veränderungen.
Eine MRT wurde zwei Wochen später durchgeführt. Zu diesem Zeitpunkt hatten sich die Symptome deutlich gebessert. Tatsächlich waren sie erstaunlich gering im Vergleich zu den auffälligen MRT-Befunden. (Vielleicht wären die MRT-Befunde eine Woche früher noch eindrucksvoller gewesen.)
Die Diagnose lautete:
Stressfraktur des Calcaneus. Natürlich wären auch andere Begriffe korrekt: „Überlastungsschaden des Knochens“, „Ermüdungsbruch“ etc.
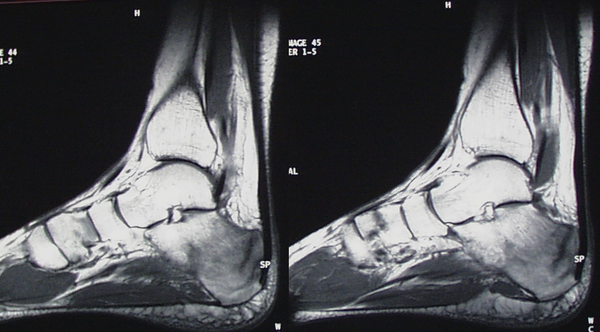
Abbildung 1b: T1
In T1 ist Fett hell, Wasser dunkel. Das Ödem verdrängt das Fettmark und macht den Knochen dunkel. T1 ist ästhetisch und liefert anatomisch klare Bilder. Pathologisches Gewebe (Ödem, Entzündung) ist meist dunkel.
STIR vs. T1: In STIR ist Wasser hell, Fett dunkel. In T1 ist Fett hell, Wasser dunkel. Beide Sequenzen zeigen dieselbe Pathologie auf gegensätzliche Weise. Das hilft bei der Abgrenzung.
Histologisch in der Remodeling-Zone: Ödem wird durch heilendes, strukturiertes Gewebe ersetzt (teils kalzifiziert). Parallel zur Heilung finden sich Zeichen von Schaden (Ödem, Nekrose, Hämatom). Knochen und Weichteile reagieren gemeinsam.
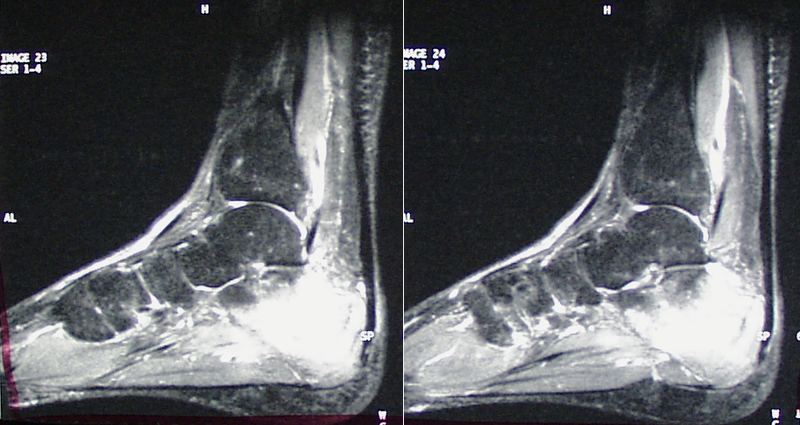
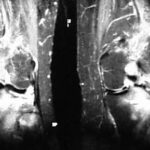
Abbildung 1c: T1 fettgesättigt nach Kontrastmittelgabe
Durch Fettunterdrückung erscheint nur noch Kontrastmittel hell – zeigt stoffwechselaktive Regionen. Der Knochenumbau ist in vollem Gange. Hell = Aktivität, Dunkel = Ruhe.
STIR und T1 fettgesättigt sehen ähnlich aus, zeigen aber unterschiedliche Inhalte: STIR = Wasser, T1-KM = Kontrastmittel. Unterschiede werden bei reiner Flüssigkeit deutlich (STIR hell, T1 dunkel).
Verlauf: Nach 2 Wochen beschwerdefrei, später vorsichtige Rückkehr zum Sport. Die Patientin hat gelernt, auf Warnsignale zu hören. Falsche Belastung (z. B. Schuhe?) war möglich. Typischer Fall von Training ohne Anpassung.
Fall 2: Typische Marschfraktur eines Mittelfußknochens
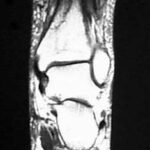
43-jährige Patientin beginnt mit täglichem Joggen. Nach vier Tagen starke Mittelfußschmerzen → Laufpause. Weichteilschwellung im Mittelfuß, sonst unauffällig. MRT angeordnet.
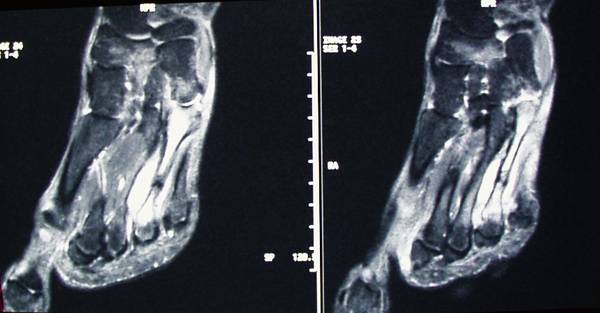

Abbildung 2b: T1, Metatarsale IV
Fettmark im gesunden Knochen hell, im pathologischen Bereich dunkel → Fett verdrängt. Diagnose: Typische Marschfraktur eines Mittelfußknochens.
Synonyme:
– Stressfraktur
– Chronisches Trauma bei gesundem Knochen
– Überlastungsschaden bei gesunden Erwachsenen
– „Insuffizienzfraktur“ bei vorgeschädigtem Knochen (z. B. Osteoporose)
Allgemeiner Begriff: Chronisches Trauma
Exakter Begriff: Ossäre Insuffizienz
Am häufigsten betroffen: 2. und 3. Metatarsale (nicht 4.). Bei Erwachsenen meist Schaft, bei Jugendlichen: Epiphyse/Wachstumsfuge.
Schmerzen sind oft verzögert, Diagnose daher schwierig. Chronische Überlastung wird leicht übersehen oder mit Tumor verwechselt.
Gesellschaftlicher Druck („Leistung ist Pflicht“) trifft Männer besonders stark – viele verletzen sich durch übermäßige Anforderungen und lehnen Therapie ab.
Guter Sportunterricht arbeitet mit Anpassung des Trainings („Training Modifikation“).
Verlauf: Beschwerden gingen mit Ruhigstellung rasch zurück. Nach 5 Wochen langsamer Trainingsaufbau ohne neue Beschwerden.
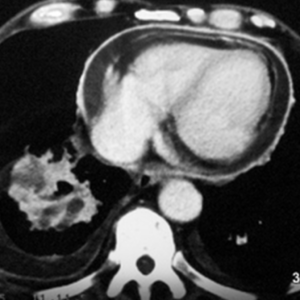
Fall 3: Osteomyelitis nach Schanz-Schraube (kein typischer Überlastungsschaden!)
Jetzt folgt ein Fall, der kein klassischer „Überlastungsschaden“ ist – aber dennoch interessant. Ähnliches wird in Artefakte II, Kapitel 5 behandelt: septische und aseptische Komplikationen nach Injektionen und Operationen. Besonders spannend ist der Vergleich zwischen STIR und T1 mit Fettunterdrückung. Wir machen einen Exkurs: von chronischem Trauma zu akutem Trauma mit entzündlicher Komplikation.
Eine 70-jährige Landwirtin erlitt eine Tibiaplateaufraktur. Eine „Schanz-Schraube“ im distalen Femur begann zu eitern und wurde entfernt. Einige Wochen später bildete sich ein Abszess im Weichteilgewebe und Knochen, der ausgeräumt und mit einer Antibiotika-Kette gefüllt wurde. Nach weiteren sechs Wochen wurde diese Kette entfernt.
Vier Monate später traten erneut starke Schmerzen und Schwellungen im distalen Oberschenkel auf – ohne sichtbare Rötung, aber mit erhöhter Temperatur (37,9 °C). Eine MRT wurde durchgeführt.

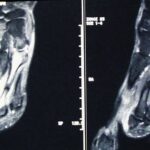
Abb. 3a–c
Es wurden drei Bilder aufgenommen:
- a. STIR (oben)
- b. T1 (mittig, ohne Fettunterdrückung)
- c. T1 nach Kontrastmittelgabe (unten, mit Fettunterdrückung)
Letzteres ist ein T1-Bild mit Fettunterdrückung und zusätzlicher Kontrastmittelanreicherung. Dadurch erscheinen alle durchbluteten Strukturen besonders hell.
Alle drei Bilder wurden in koronaler Schichtführung aufgenommen. Die Merkmale ähneln stark denen in den Fällen 1 und 2.
Der Knochendefekt ist im STIR klar erkennbar. Er ist nun teilweise durch dunkles und teilweise durch helles Gewebe ersetzt. Was sowohl im STIR als auch im T1 mit Kontrastmittel hell erscheint, ist durchblutetes Gewebe. Im Inneren befindet sich Flüssigkeit: In STIR erscheint sie hell, in T1 (mit und ohne KM) jedoch dunkel. Dies spricht für Eiter – also einen Abszess.
Auf den ersten Blick sieht das T1-Bild mit Kontrastmittel dem STIR-Bild ähnlich: Auch hier ist die Muskulatur dunkel, das ursprünglich helle Fett wurde durch Fettunterdrückung ebenfalls dunkel. Doch: STIR und T1 mit Kontrastmittel (und Fettunterdrückung) unterscheiden sich in der Interpretation deutlich.
Flüssiger Eiter – das nicht durchblutete Zentrum der Läsion – ist in STIR hell, in T1 dunkel.
Damit erlaubt das letzte Bild eine differenzierte Beurteilung von:
- Abszessmembran (entzündlich aktiviertes Gewebe, gut durchblutet)
- Abszesshöhle (nicht durchblutete Flüssigkeit – Eiter)
Beide Komponenten waren im STIR sichtbar, aber nicht unterscheidbar.
Dieser Fall zeigt den zusätzlichen diagnostischen Wert von Kontrastmittel (KM). Es erlaubt eine spezifischere Differenzierung als STIR allein:
- T1 mit KM: Zentrum = dunkel, Rand = hell → gut unterscheidbar
- STIR: Zentrum & Rand = hell → nicht unterscheidbar
Der nächste Fall führt zurück zum Thema „chronisches Trauma“.
Fall 4: Stressfraktur der distalen Tibia

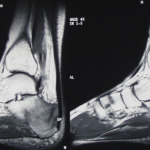
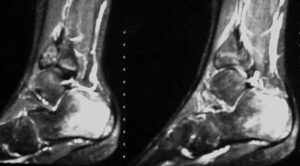
Abb. 4a – STIR (Short Tau Inversion Recovery)
Ein 56-jähriger Zahnarzt unternahm zweieinhalb Wochen vor der MRT eine sehr anstrengende Wanderung. Er musste wegen Regen umkehren, verirrte sich, und war so einer ungewöhnlichen Belastung ausgesetzt. Wenige Stunden nach seiner Rückkehr verspürte er starke Schmerzen im distalen Unterschenkel.
Die Schwellung und Überwärmung der Weichteile verwirrten selbst den behandelnden Arzt. Da das Röntgenbild unauffällig war, wurde bei der Verdachtsdiagnose „Arthritis eines Einzelgelenks?“ oder „Tumor?“ eine MRT veranlasst. Dass dabei die Krankengeschichte übersehen wurde, ist bemerkenswert. Links im Bild ist die STIR-Sequenz zu sehen.
Es gibt mindestens drei auffällige Merkmale:
- Der Talus ist nicht betroffen, ebenso wenig die gelenknahen Tibiaabschnitte. Bei Arthritis wäre ein helles Signal (Ödem) auf beiden Seiten des Gelenkspalts zu erwarten.
- Eine besonders helle Linie zieht sich diagonal durch die distale Tibia – hier scheint sich besonders viel Wasser (oder Blut) zu befinden.
- Die Weichteile, normalerweise dunkel im STIR, sind ebenfalls sehr hell – pathologisch besteht ein massives Ödem.
Im STIR erkennt man eine empfindliche Hervorhebung des starken Muskelödems. Dieses setzt sich über einen Kortikalisdefekt in das Knochenmark fort. Ob es sich dabei um Flüssigkeit oder entzündliches Gewebe handelt, bleibt unklar.
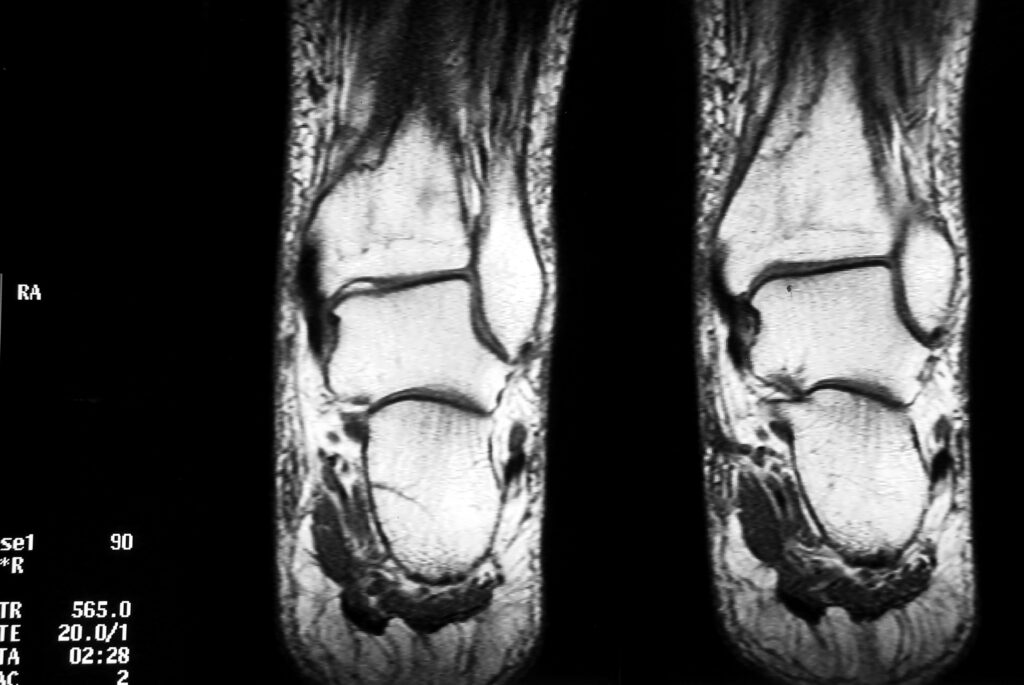
Abb. 4b – T1 (klassische Spin-Echo-Sequenz)
T1-gewichtete Sequenzen unterscheiden sich deutlich vom STIR: In T1 erscheint Fett sehr hell, freie Flüssigkeit (z. B. Liquor, Urin, langsames Blut) dagegen dunkel. Die hohe Auflösung eignet sich gut zur anatomischen Darstellung.
Wer glaubt, STIR durch T1 ersetzen zu können, irrt: Pathologien erscheinen in T1 oft nur leicht dunkler als gesundes Gewebe – und werden daher leicht übersehen. Besonders kritisch sind Fälle, in denen das STIR ein sehr helles Signal zeigt, T1 aber nur eine schwache Abdunklung. Je nach Bildfensterung kann diese sogar ganz untergehen.
Die Subkutis (Fettgewebe unter der Haut) ist normalerweise sehr hell in T1. Hier ist sie ödematös infiltriert; das Erscheinungsbild ist ungleichmäßig mit hellen Knoten und dunklem Netzwerk – Flüssigkeit zwischen den Fettläppchen.
Im Bereich der distalen Tibia ist das Signal schwächer, weil Fettmark durch Flüssigkeit verdrängt wurde (Stressfraktur). Die Abdunklung ist nicht sehr deutlich, was die Diagnose erschwert.
Entlang einer schrägen Linie ist das Fettsignal besonders reduziert – das entspricht der dunklen Frakturlinie.
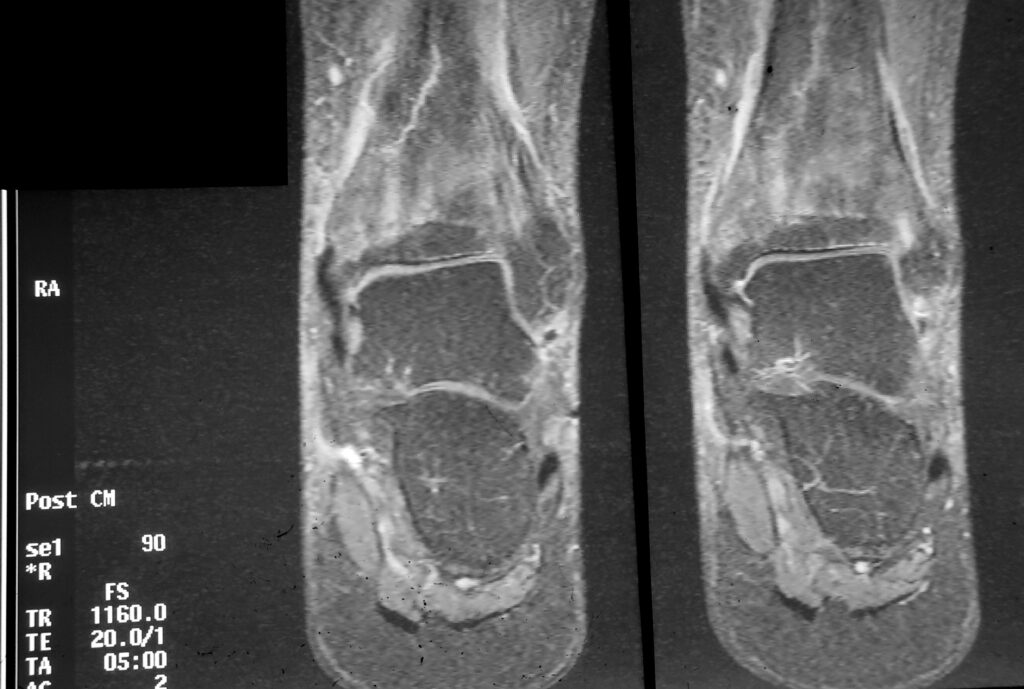
Abb. 4c – T1 fettgesättigt nach Kontrastmittelgabe
Das dritte Bild (Abb. 4c) basiert wie Bild b auf einer T1-Sequenz, unterscheidet sich aber deutlich. Es wurde nach intravenöser Kontrastmittelgabe aufgenommen und enthält Fettunterdrückung.
Nur T1-Bilder zeigen Kontrastmittel. Da aber sowohl Fett als auch KM hell erscheinen, stört das die Bildinterpretation. Fettunterdrückung löst dieses Problem: Fett wird dunkel, KM bleibt hell. So sieht man deutlich die Verteilung des Kontrastmittels.
Im aktuellen Fall gibt es keine Hinweise auf synoviale Proliferation, wie sie für Arthritis typisch wäre. Stattdessen findet sich eine unregelmäßige, gestreifte KM-Anreicherung in der distalen Tibia. Weiter unten – über dem Sprunggelenk – ist eine ungewöhnliche Knochenstruktur erkennbar.
Dort, wo das KM besonders deutlich sichtbar ist, besteht ein „heißer“ Stoffwechselprozess – typisch für eine reparative Reaktion. Innerhalb der Heilungszone erkennt man eine schräge, helle Linie – Ausdruck einer gesteigerten Durchblutung. Die Form und Struktur sprechen nicht für eine tumorartige Veränderung.
Es handelt sich um einen klassischen Überlastungsschaden.
Die Fehleinschätzung des zeitlichen Zusammenhangs zwischen Beschwerden und vorangegangener Überlastung ist bemerkenswert. Es wurde übersehen, dass Knochen Zeit braucht – sowohl zur Reaktion als auch zur Heilung. Ebenso wurde nicht erkannt, dass Überlastungsschäden sich auch in angrenzenden Weichteilen manifestieren.
Das gilt für alle acht beschriebenen Formen von Überlastungsschäden (siehe Artikel 01): akutes oder chronisches Trauma, wachsender oder ausgereifter Knochen, gesunder oder vorgeschädigter Knochenstoffwechsel. Jede Kombination ergibt eine eigene „Osteopathie“-Konstellation.
Fall 5: Enthesopathien
Enthesopathien stehen in engem Zusammenhang mit Stressfrakturen. Im weiteren Sinne handelt es sich um „sterile Entzündungen“ der Sehnen, verursacht durch Fehlbelastung.


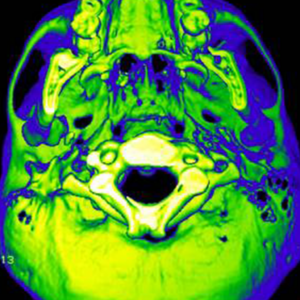
Abbildung 5a + 5b: koronare Schnitte; STIR und T1 ohne Fettunterdrückung
Abbildung 5c: T2* sagittal
Ein 28-jähriger Sportler hatte über fünf Wochen hinweg intensiv trainiert. Allmählich zunehmende Schmerzen in beiden Achillessehnen wurden schließlich so stark, dass er nur noch unter Schmerzen auf den Zehenspitzen stehen konnte. Gleichzeitig bemerkte er eine lokale Schwellung der Achillessehnen auf beiden Seiten.
Unterhalb des STIR-Bildes (unten rechts) ist eine normale T1-Sequenz zu sehen. Sehne und Flüssigkeitseinlagerung erscheinen dunkel und sind daher schwer zu unterscheiden. Die Auflösung ist jedoch gut und die Anatomie klar erkennbar. Die pathologische Veränderung der Achillessehne ist deutlich sichtbar.
Abbildung 5c zeigt eine T2*-Gradientenechosequenz in sagittaler Schichtung. Diese Sequenz hat T2-Charakteristika: Flüssigkeit – und damit nahezu jedes pathologische Gewebe – erscheint hell. Fett ist mäßig hell, weniger als in T2-Spin-Echo, deutlich schwächer als in T1. Im Gegensatz zu STIR wird das Fettsignal hier nicht unterdrückt.
Was sind die Hauptunterschiede zwischen T1 und T2?
Erhöhte Flüssigkeit (also fast alle Pathologien): dunkel in T1, hell in T2.
Was haben T1 und T2 gemeinsam?
Fett erscheint hell – allerdings in T1 deutlich heller.
Eine der wenigen Substanzen, die sich im MRT ähnlich wie Fett verhalten, ist Met-Hämoglobin.
Die Regel der Fettabbildung gilt nicht uneingeschränkt: Verschiedene T2-Sequenzen unterscheiden sich im Fettsignal. Diese Unterschiede ermöglichen uns diagnostische Differenzierungen. In manchen Fällen ist ein gedämpftes Fettsignal nicht erwünscht – z. B. bei Lymphknoten oder Knochenmetastasen, die sich sonst im umgebenden Fett „verstecken“ könnten. Im Vergleich zu T2-Spin-Echo und Turbo-Spin-Echo unterdrückt T2*-Gradientenecho das Fett stärker.
Die einfachste Ausgangsbasis ist eine klassische Spin-Echo-Sequenz: Sie unterdrückt Fett kaum und hat ein deutlich helles Fettsignal (T1: sehr helles Fett).
Dieses Beispiel zeigt die Eignung der T2*-Gradientenecho-Sequenz: Durch die Fettunterdrückung wird das helle Signal der pathologischen Flüssigkeitseinlagerung in der Achillessehne sehr deutlich. Die Muskulatur erscheint in allen T2-Sequenzen eher dunkel. Wir haben diese Hervorhebung der Pathologie bereits im STIR gesehen.
Hat T2* Vorteile gegenüber STIR?
Ja – nicht in der Gewebe-Differenzierung, sondern in der besseren Detailauflösung und der höheren Messgeschwindigkeit.
Case 6: Acute trauma with infraction of the tibial plateau; (i.e. not chronic but acute overuse damage)
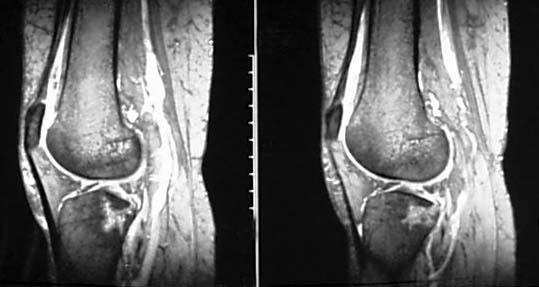
Abb. 6a
Abb. 6 a + b; sagittale Ansicht; T2*
Dies ist ein 43-jähriger Mann, der vor fünf Tagen aus zwei Metern Höhe von einem Gerüst gestürzt ist.
Zunächst ist wichtig zu erwähnen, dass das Röntgenbild keine pathologischen Befunde zeigte. – Der Patient hatte jedoch (fünf Tage nach dem Unfall) weiterhin starke Schmerzen beim Laufen, Stehen, bei Belastung des Kniegelenks sowie bei Valgusstress. Eine kleine blutige Gelenkerguss wurde punktiert. Aufgrund der Ergebnisse dieser Punktion und der anhaltenden Symptome wurde eine MRT-Untersuchung angeordnet.
Wir verweilen nicht bei der Beschreibung der MRT-Bilder, sondern interpretieren die Befunde pathophysiologisch: Es zeigt sich ein ausgedehntes Knochenmarködem im lateralen Tibiaplateau. Oben sind zwei verschiedene T2*-Schnitte dargestellt. Es zeigt sich ein ausgeprägtes Knochenmarködem im dorsalen Tibiaplateau. Dieses Ödem ist im unteren (rechten) Bildpaar noch deutlicher sichtbar. Es handelt sich um eine Sequenz, die das Fettgewebe stark unterdrückt und gleichzeitig die „pathologische Flüssigkeit“ hervorhebt: Die STIR-Sequenz (unteres Bildpaar).
Vor dem Hintergrund dieser Anamnese suchen wir nach direkten Frakturzeichen: Es gibt keinen Hinweis auf eine Eindellung der Gelenkfläche der Tibia. Das ausgeprägte Knochenmarködem im Tibiaplateau wird in beiden gezeigten Sequenzen (und in beiden Schnittführungen) von einer Niedrigsignal-Linie durchzogen. Dies ist wahrscheinlich auf eine trabekuläre Kompression zurückzuführen, die das helle Signal aus dem Markraum reduziert. Eine Röntgenuntersuchung wie eine Computertomografie (CT) könnte diese Hypothese stützen. Auch ohne CT ist die Diagnose durch die Summe aus Sequenzen und Anamnese eindeutig:
Es handelt sich um eine Infraction des lateralen Tibiaplateaus.
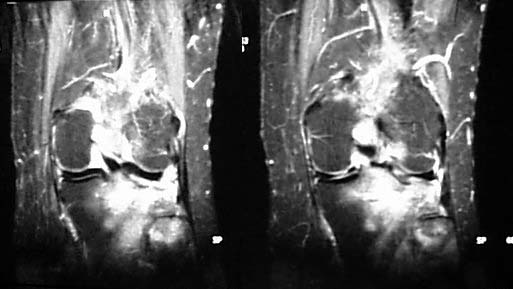
Abb. 6b
Abb. 6b STIR. Dieses Ödem ist noch deutlicher sichtbar in einer Sequenz, die Fettgewebe stark unterdrückt und „pathologische Flüssigkeit“ hervorhebt.
Es wurde eine konservative Behandlung mit teilweiser, aber konstanter Entlastung gewählt. – Eine komplexe und teure MRT ist sinnvoll, da sie zeigt, dass dieses verletzte Areal gefährdet ist. Wenn die Belastung nicht reduziert wird, könnte sich hier ein Bluterguss bilden, was vermutlich zu bleibenden Gelenkschäden führen würde.
Tatsächlich war der Patient nach wenigen Tagen beschwerdefrei. Nach vier Wochen kehrte er an seinen Büroarbeitsplatz zurück.
Die Röntgenkontrolle nach vier Monaten zeigte unauffällige Befunde, also normale Knochen- und Weichteilstruktur im Tibiaplateau und normale Gelenkspaltweite.
Fall 7: Überlastungsschaden des Os cuboideum
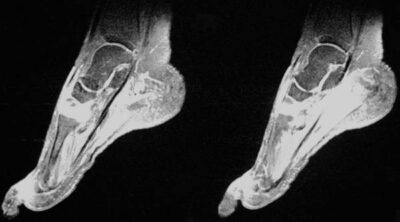
Abb. 7 a + b: STIR
Ein (atypisch lokalisierter) Überlastungsschaden wurde vermutet.
Weitere Diagnostik ergab einen deutlich reduzierten Dichtemesswert in der quantitativen CT des Radius. Im Femur und der Wirbelsäule fanden sich jedoch Normalwerte. Diagnose: Atypische periphere Osteoporose.
Die Überlastung des Fußskeletts traf somit auf krankhaft veränderten Knochen und war daher besonders wirksam (und das an einer atypischen Stelle).
Die Beschwerden besserten sich kontinuierlich, aber es dauerte fünf Monate bis zur vollständigen Beschwerdefreiheit.
Kurz nach dem Abklingen der Beschwerden verspürte die Patientin nach erneuter Belastung Schmerzen im Fußwurzelbereich der Gegenseite. Eine Bildgebung wurde nicht durchgeführt.
Drei Monate später erlitt sie nach einem Sturz eine typische Fraktur des rechten distalen Radius. Zwei Jahre zuvor hatte sie sich bei einem Sturz drei Mittelhandknochen gebrochen. – Es kann davon ausgegangen werden, dass eine Prädisposition für akute und chronische Traumata vorliegt. Die häufigste Ursache für eine solche „ossäre Insuffizienz“ ist Osteoporose.
Die Patientin wurde mit Calcium und Vitamin D behandelt. Nach über einem Jahr geht es ihr gut. Es traten keine neuen Überlastungsschäden oder akute Frakturen mehr auf. Es gibt weiterhin keinen Hinweis auf eine rheumatologische Erkrankung. Es bestand nie ein Hinweis auf Hyperparathyreoidismus oder Osteomyelitis.
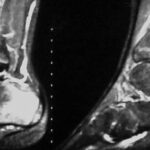
Fall 8. Schädigung beider Fersenbeine (Calcanei) eines jungen Menschen durch Überlastung
Der 12-jährige Patient ist ein sehr aktiver Fußballspieler. Nach einer Reihe sehr intensiver Trainingstage entwickelte er plötzlich Schmerzen in beiden Fersen. Dies zwang ihn, mit dem Sport aufzuhören. Ein Unfall wurde ausgeschlossen. – Als die Schmerzen auch nach mehreren Tagen bei leichter Belastung anhielten und das Röntgenbild nur alterstypische Befunde zeigte, wurde eine MRT durchgeführt.
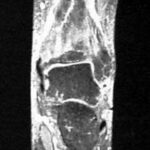
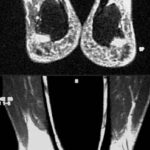
Abb. 8 a – d: MRT sagittal beider Fersenbeine
Was zeigte die MRT bei unserem Patienten? Es bestand ein ausgedehntes Knochenmarködem beider Calcanei. Beide Bildpaare sind T2*-Gradientenechosequenzen. Beide Fersen sind dargestellt (oben: linker Calcaneus; unten: rechter Calcaneus).
Die pathologischen Befunde zeigen eine bemerkenswerte Symmetrie: es besteht ein ausgedehntes Knochenmarködem der Apophysenkerne und der metaphysären Anteile nahe der Wachstumsfuge.
Bemerkenswert ist, dass sowohl der in diesem Alter bereits große Apophysenkern als auch die Wachstumsfuge und die metaphysären Anteile in unmittelbarer Nähe der Wachstumsfuge betroffen sind. Auch die normale Wachstumsfuge zeigt ein erhöhtes Signal, das jedoch deutlich über dem altersphysiologischen Niveau liegt.
Diese Lokalisation ist typisch für eine Schädigung des wachsenden Skeletts. Es handelt sich höchstwahrscheinlich um eine Vorstufe oder sehr frühe (reversible) Form einer aseptischen Nekrose.
Bei konsequenter Schonung verheilte diese Veränderung spurlos.
Würden die Veränderungen fortschreiten, wäre zu erwarten, dass der Apophysenkern aufgrund von Wachstumsfugenschwäche nekrotisch wird und sich verlagert. Ebenso wäre zu erwarten, dass sich die ebenfalls betroffene Metaphyse an diesen verlagerten Kern anpasst – im Rahmen des Reparaturprozesses.
Je nach Betrachtungsweise ergeben sich verschiedene Bezeichnungen:
Röntgenologisch sieht es aus wie eine Apophysitis.
Histologisch lässt sich der Befund als aseptische Nekrose einordnen.
Pathogenetisch handelt es sich um einen typischen Überlastungsschaden im Jugendalter.
Auffällig bei all diesen Fällen von „ossärer Insuffizienz“ ist, dass sie leicht durch das Raster der medizinischen Fachgebiete fallen. Der Chirurg sagt: „Was soll ich mit diesem Patienten anfangen?”

Abb. 8a
Abb. 8b

Abb. 8c
Abb. 8d
Liebe Leser:innen!
Einige von Ihnen sind auf diese Seite gekommen, weil Sie etwas zur Wachstumsfuge gesucht haben. Der hier gezeigte Fall ist, was die Wachstumsfuge betrifft, ein sehr schwieriges Problem. Dieser Fall eignet sich nicht als Einstieg. Ganz kurz: Wir wachsen in den Wachstumsfugen. Sie trennen den Kern (Epiphyse/Apophyse) vom Schaft (Metaphyse). Wenn wir aufhören zu wachsen, verschmelzen sie miteinander und die Fuge verschwindet.
Es ist leicht vorstellbar, dass eine solche Zone einer sehr komplexen „Knochenstruktur“ besonders empfindlich ist gegenüber Überlastung. Ein solcher Fall ist hier beschrieben.
Ein anderer Artikel befasst sich mit der Wachstumsfuge:
Artefakte III, Kapitel 7, Abbildung 05. Es kann vorkommen, dass diese W. sich nicht schließen, sondern auch im Erwachsenenalter noch im Röntgen sichtbar bleiben. Dies wurde als Ausdruck eines gelenknahen Prozesses an der Wirbelsäule gedeutet.
Würden die Veränderungen fortschreiten, dann erwarten wir, dass der Apophysen-Kern nekrotisch wird und die Wachstumsfuge nicht mehr einen ausreichenden Halt bietet. Der Kern könnte sich dann verschieben. Wir dürfen hoffen, dass das Ganze doch nochmal abheilt, aber dann unter einer Verformung.
Weiterhin wäre zu erwarten, dass sich die ebenfalls betroffene Metaphyse – im Zuge reparativer Vorgänge – an diesen verlagerten Wachstumskern adaptiert. Auch das bedeutet nach der Ausheilung eine Formveränderung. Diese mag für die Funktion mehr oder weniger bedeutsam sein.
Je nach der Betrachtungsweise resultieren verschiedene Benennungen:
Röntgenologisch erwarten wir also das Bild einer Apophysitis.
Histologisch wird diese Erkrankung in die aseptischen Nekrosen einzuordnen sein.
Von der Pathogenese ist es ein typischer Überlastungsschaden im jugendlichen Alter.
Bei allen diesen Fällen von “ossärer Insuffizienz” ist auffällig, dass sie leicht durch das Raster der medizinischen Diszipline fallen. Der Chirurg sagt: „Was soll ich mit diesem Patienten anfangen, der hatte ja gar keinen Unfall.“ Der Rheumatologe sagt: „Keine Entzündungsparameter!“ Fühlt sich der Orthopäde angesprochen?
Allen Kolleg:innen fallen bei diesen Patienten psychologische Besonderheiten auf. Die Patienten sind getroffen; ihr Krankheitsgefühl ist oft ausgeprägt. Andererseits fehlt auch oft die Einsicht, dass die Therapie möglicherweise einfach ist.
Es sind erfreulicherweise sehr gutartige Erkrankungen. Daher sei den Kasuistiken ein Ausblick in die besondere Psychodynamik angehängt.
9.
Psychodynamisches Modell der Überlastungsschäden in Stichworten
Fokus auf Sporttrauma in der zweiten Lebenshälfte.
Überlastungsschäden entstehen durch ein Missverhältnis zwischen Belastung und Widerstand. Belastung hat ihre eigene Psychodynamik. Die wirkenden Faktoren lassen sich in endogene und exogene einteilen.
- Endogene Faktoren
1.1. Persönlichkeitsmerkmale.
- Bei Verdacht auf Überlastungsschäden sollte nach narzisstisch gestörten Anteilen in der Persönlichkeit gesucht werden. Kennzeichnend ist ein gesteigertes Grandiositätsempfinden in Vorstellung und Verhalten: Übertriebenes Gefühl der Besonderheit („etwas Einmaliges“); Aufgehen in Fantasien von Macht und/oder Schönheit; gesteigertes Bedürfnis nach Bewunderung.
- Mangelndes Selbstgefühl: Aufgrund mangelnder Körperwahrnehmung wird der Körper nur in Grenzsituationen oder bei deren Überschreitung gespürt. Das heißt, die Gefühle in der Grenzsituation (z. B. Schmerz) sensibilisieren nicht zur Vorsicht, sondern fördern eine Übersteigerung der eigenen Leistungsfähigkeit.
- Mangelnde Konfliktlösungsfähigkeit. Konflikte werden mitunter autoaggressiv durch körperliche Abreaktion zu bewältigen versucht.
1.2. Umgang mit dem Altern. Übermäßige Angst vor Altern, körperlicher Schwäche, Krankheit und letztlich Angst vor dem Tod. Die Abwehrmechanismen dieser Angst sind:
- a) – Verdrängung („Ich bin doch noch jung! Ich kann ruhig zehn Kilometer am Tag joggen!“)
- b) – Verleugnung („Älterwerden betrifft mich nicht! Was haben die alle mit dem Alter? Zwei Stunden Tennis täglich, das brauche ich!“)
- c) – Projektion
(„Sieh dir diesen Schwächling da an! Ich bin gut, weil alle um mich herum so schwach und jammernd sind. Wenn ich mich mit ihnen vergleiche, merke ich, wie stark ich bin! Wer mich sieht, muss sich minderwertig fühlen!“) 2. Exogene Faktoren
2.1. In der kulturell geprägten Sichtweise unserer Gesellschaft werden Jugend, körperliche Fitness und äußere Schönheit hoch bewertet. Dies wird insbesondere durch Werbung vermittelt und konkretisiert. Um erkennbar zu bleiben und sich vom „Altsein“ abzugrenzen, versuchen ältere Menschen, diesem Bild körperlicher Fitness zu entsprechen. Der Verlust körperlicher und geistiger Leistungsfähigkeit wird nicht als natürlicher Prozess akzeptiert, sondern ausgeklammert und höchstens als pathologische Ausnahme toleriert. Es entwickeln sich Wettbewerbssituationen, in denen ältere Menschen mit Jüngeren konkurrieren wollen („… jetzt zeig ich euch mal, was ich noch drauf hab“). Das führt zu Überlastungen. Die neuen Sportarten, die in den letzten zwei Jahrzehnten entstanden sind, bieten viele Möglichkeiten zur Leistungsdarstellung und -vermessung. Dazu zählen auch Extremsportarten, die den notwendigen „Kick“ liefern. Es handelt sich vermutlich auch um den Versuch, die Wirkung von Endorphinausschüttung in Extremsituationen oder bei extremer körperlicher Belastung immer wieder zu spüren. Die Übergänge zu suchtähnlichem Verhalten sind fließend.
Therapeutische Optionen. Die Umsetzbarkeit einer Therapie hängt von der Einsichtsfähigkeit in die Störung und der Fähigkeit zur Introspektion ab. Diese sind häufig unzureichend. Das Trauma wird oft als schicksalhaft erlebt. Das Selbstbild erlaubt keine Einsicht in eigenes Fehlverhalten. Das Trauma erscheint dem Patienten als äußeres Unglück. Es besteht kein Bewusstsein dafür, dass er selbst die Ursache sein könnte. Es fehlt an Eigenverantwortung für das Trauma, die Ursachen werden nach außen projiziert.
Selbst bei mangelnder Krankheitseinsicht gibt es verschiedene therapeutische Möglichkeiten:
– Der suggestive Effekt von Medikamenten. („Solange dieses Knochenmarködem besteht, ist eine Trainingspause unbedingt notwendig, um weitere Schäden zu vermeiden!“ Der „Bone Bruise“ muss sprechen, statt der schwachen Introspektion.)
– Weitere therapeutische Ansätze beinhalten verhaltensverändernde Interventionen:
- Ansprache der narzisstischen Persönlichkeitsanteile zur Verringerung des Bewunderungsbedarfs. („Du musst dich nicht so reinhängen.“)
- Lernen am Modell. Relativierung und Modifikation des durch Werbung vermittelten Persönlichkeitsbildes („Weißt du, wie ich Sport mache – ich mach das so und so. Es bringt mir nichts, wenn ich mich kaputt mache.“)
Bei ausreichender Therapiebereitschaft und Einsicht in die Störung:
– Tiefenpsychologischer Zugang zur Auseinandersetzung mit primären familiären Ursachen, z. B. Bewusstmachung mangelnder elterlicher Anerkennung oder Aufmerksamkeit, Hinterfragen der Verknüpfung zwischen Zuwendung und bestimmten Leistungen. Anerkennung nur dann, wenn man „besser“ ist als andere usw.
– Körpertherapeutisch orientierter Therapieansatz durch „sanfte Therapiemethoden“ wie Körperwahrnehmungstraining, körperbezogene Entspannungstechniken (Muskelentspannung nach Jacobson, autogenes Training nach Schultz).
Unser einführender und fortbildender Artikel endet hier. Wenn Sie Anregungen haben, teilen Sie sie uns gerne mit. Die E-Mail-Adressen finden Sie ganz unten.
Wenn Sie Anregungen oder Fragen haben, wenden Sie sich bitte an:
Schmittbuxbaum(at)gmail.com oder wghschmitt(at)gmx.de
Ein weiterer Artikel zum Thema „Ossäre Insuffizienz“ ist der vorherige, 01.